Basal Cell Carcinoma: The Hidden Skin Threat You Need to Know About
Skin cancer is a growing concern worldwide, with basal cell carcinoma (BCC) being the most common type. Often overlooked due to its slow-growing nature, BCC can cause significant damage if not treated promptly. As a medical dermatologist, I aim to shed light on this pervasive condition, providing crucial insights and answering frequently asked questions.
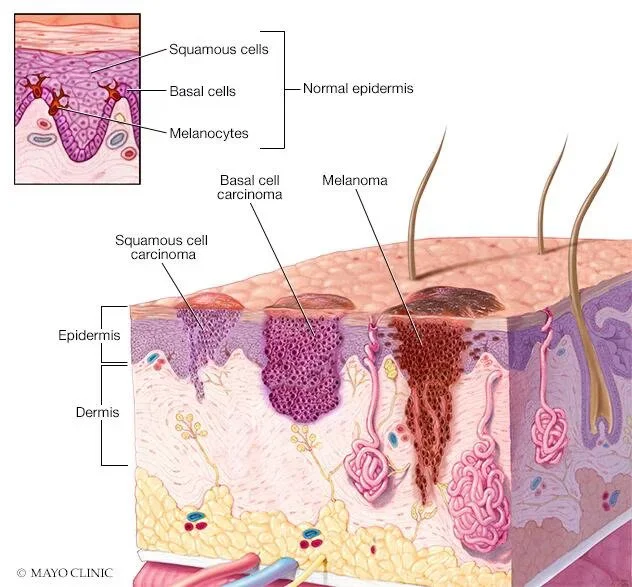
Understanding Basal Cell Carcinoma
Basal cell carcinoma originates in the basal cells, which are located in the deepest layer of the epidermis. It typically develops in areas exposed to the sun, such as the head, neck, and arms. Unlike other forms of skin cancer, BCC rarely metastasizes (spreads to other parts of the body). However, it can be locally invasive, leading to significant tissue damage and disfigurement.
Recognizing the Symptoms
Early detection of BCC is critical for effective treatment. Here are common signs to watch for:
Pearly or Waxy Bumps: These often appear on the face, ears, or neck and may have visible blood vessels.
Flat, Flesh-Colored Lesions: Typically found on the back or chest, these lesions can be brown or skin-colored.
Sores That Don’t Heal: Persistent sores that bleed, ooze, or crust over could indicate BCC.
Scar-Like Lesions: White, waxy scars without a clear history of injury may also be a warning sign.
Causes and Risk Factors
The primary cause of BCC is prolonged exposure to ultraviolet (UV) radiation from the sun or tanning beds. UV radiation damages the DNA in skin cells, leading to mutations that result in cancer. Several factors increase the risk of developing BCC:
Fair Skin: Individuals with light skin, blue or green eyes, and blond or red hair are more susceptible.
History of Sunburns: Severe, blistering sunburns during childhood or adolescence can heighten the risk.
Age: BCC is more common in older adults, as the cumulative exposure to UV radiation increases over time.
Family History: A family history of skin cancer can indicate a genetic predisposition.
Immune Suppression: Conditions or medications that weaken the immune system can elevate the risk.
Treatment Options
The treatment of basal cell carcinoma depends on the size, location, and depth of the tumor. Common treatment methods include:
Surgical Excision: The tumor is cut out along with a margin of healthy tissue. This is the most common treatment.
Mohs Surgery: This precise surgical technique removes the cancer layer by layer, examining each layer under a microscope until no abnormal cells remain. It’s particularly useful for recurrent BCC or those in cosmetically sensitive areas.
Cryotherapy: The tumor is frozen using liquid nitrogen. This is effective for superficial BCC.
Topical Treatments: Creams and ointments containing imiquimod or 5-fluorouracil can be used for small, superficial BCCs.
Radiation Therapy: This is an option for patients who cannot undergo surgery.
Prevention Strategies
Prevention is the best defense against basal cell carcinoma. Here are some tips to reduce your risk:
Sun Protection: Apply a broad-spectrum sunscreen with an SPF of 30 or higher, even on cloudy days. Reapply every two hours, or more often if swimming or sweating.
Avoid Tanning Beds: Artificial UV radiation from tanning beds is just as harmful as the sun.
Wear Protective Clothing: Long-sleeved shirts, wide-brimmed hats, and sunglasses can provide additional protection.
Seek Shade: Stay out of the sun during peak hours, usually from 10 a.m. to 4 p.m.
Regular Skin Checks: Perform self-examinations monthly and schedule annual skin exams with a dermatologist.
Impact of Basal Cell Carcinoma on Daily Life
Living with BCC can affect your daily life, especially if the carcinoma is located in visible areas like the face or neck. The psychological impact can be profound, leading to self-consciousness and anxiety about appearance. In addition, treatments can be time-consuming and may require multiple visits to the dermatologist, causing disruptions in personal and professional life. However, with the right care and support, many patients can manage these challenges effectively.
The Role of Dermatologists in Managing BCC
Dermatologists play a crucial role in the early detection and treatment of BCC. Regular check-ups allow for the monitoring of skin changes and prompt action when abnormalities are detected. Dermatologists also educate patients on the importance of sun protection and healthy skin practices, which are vital in preventing BCC and other skin conditions. Their expertise ensures that patients receive the most appropriate and effective treatments available.
FAQs About Basal Cell Carcinoma
1. Can basal cell carcinoma spread to other parts of the body?
While BCC rarely metastasizes, it can invade surrounding tissues and cause significant local damage. Early detection and treatment are crucial to prevent complications.
2. How is basal cell carcinoma diagnosed?
Diagnosis typically involves a physical examination and a biopsy. During a biopsy, a small sample of the suspicious lesion is removed and examined under a microscope.
3. What is the recovery time after treatment for basal cell carcinoma?
Recovery time varies depending on the treatment method. Surgical excision and Mohs surgery may require a few weeks for healing, while topical treatments and cryotherapy might have shorter recovery periods.
4. Is basal cell carcinoma hereditary?
While BCC itself is not directly inherited, a family history of skin cancer can indicate a higher risk. Genetic factors, combined with environmental exposure, contribute to the development of BCC.
5. Can basal cell carcinoma recur after treatment?
Yes, BCC can recur, especially if the initial tumor was large or not completely removed. Regular follow-up appointments with a dermatologist are essential to monitor for any signs of recurrence.
6. What should I do if I notice a suspicious skin lesion?
If you observe a suspicious skin lesion, such as a new growth, a sore that doesn't heal, or a change in an existing mole or spot, it's important to consult a dermatologist as soon as possible. Early diagnosis and treatment are key to managing BCC effectively.
7. Are there lifestyle changes I can make to reduce my risk of developing BCC?
Yes, adopting sun-safe behaviors is crucial. This includes using sunscreen daily, wearing protective clothing, avoiding peak sun hours, and steering clear of tanning beds. Additionally, maintaining a healthy lifestyle with a balanced diet and regular exercise can support overall skin health.
Conclusion
Basal cell carcinoma, though common, should not be taken lightly. Awareness, early detection, and proactive prevention are key to managing this form of skin cancer. By understanding the risk factors, symptoms, and treatment options, you can take the necessary steps to protect your skin and overall health. Always consult with a dermatologist if you notice any suspicious changes in your skin, and prioritize regular skin examinations to catch potential issues early. With the right knowledge and actions, you can significantly reduce your risk and ensure a healthier future for your skin.